A 30 year old male
This is an online e-log platform to discuss case scenario of a patient with their guardians permission.
I have been given this case to solve in an attempt to understand the topic of patient clinical data analysis to develop my competency in reading and comprehending clinical data including histoty, clinical findings, .investigations and come up with a diagnosis and treatment plan.
DANDU SHIVANI.
INTERN
A 30 year old male patient resident of Gudipally came to the casualty on 23/11/22 of altered behaviour since yesterday
Involuntary micturition since yesterday
Giddiness since morning
HOPI.
Patient was apparently asymptomatic till 12 am last night then he started behaving abnormally which was sudden in onset in terms of not .responding when spoken to,irrelevant talk which is repetitive and self talking.patient is irritable every few minutes and abuses family members at times.
Patient had history of alcohol consumption since 10 years currently 6 to 10 units daily throughout day,reports craving for alcohol, sweating and trembling when he doesn't consume alcohol.patient stopped consumption for the past 10 days till yesterday but was given 3 units I/v/o tremors
@ 10:30 am which subsided after consumption . patient.also reported double images and slurring of speech and memory disturbances since 10 days.patient reports consumption of tobacco in the form of smoking(10 cigarettes per day).
PAST HISTORY
H/O fall 1 month back ,sustained injury @ head.
N/K/C/O DM,HTN, TB ASTHAMA, EPILEPSY.
FAMILY HISTORY: not significant
PERSONAL HISTORY
DIET: Mixed
APPETITE: decreased
SLEEP: disturbed
BOWEL AND BLADDER MOVEMENTS: regular
ADDICTIONS: alcoholic since 10 years.
ON EXAMINATION.
Patient is conscious.
No signs of pallor, icterus, cyanosis, clubbing, lymphadenopathy,edema.
Temperature
BP: 120/80 mm hg
PR:68/min
RR:18/ min
SPO2:98% at room air.
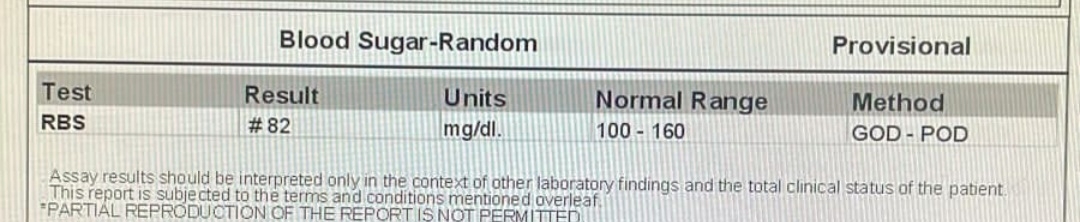
GRBS: 98MG/DL.
SYATEMIC EXAMINATION
CNS.
HMF: orientation to place and person present and to time absent.
MEMORY: IMMEDIATE:
SHORT TERM.
LONG TERM:
PUPILS: NSRL
SPEECH: normal.
CRANIAL NERVE EXAMINATION: INTACT
SENSORY SYSTEM NORMAL
MOTOR SYSTEM
RIGHT. . LEFT
TONE. UL Normal normal
LL. Normal. normal
POWER. UL. 4/5. 4/5
LL. 4/5. 4/5.
REFLEXES. RIGHT. LEFT
BICEPS. 2+. 2+
TRICEPS. 2+. 2+
SUPINATOR. 2+. 2+
KNEE. 2+. 2+
ANKLE. 2+. 2+
PLANTAR. 2 +. 2+
SENSORY SYSTEM: normal.
CEREBELLAR SIGNS
FINGER NOSE TEST - IN COORDINATION PRESENT
FINGER FINGER TEST- IN COORDINATION PRESENT
ROMBERGS - NEGATIVE
DYSDIADOKINESIA- NEGATIVE
GAIT - NORMAL
CVS examination:
S1, S2 are heard.
No murmurs.
Respiratory system examination:
Inspection: Chest is moving bilaterally symmetrical. No pulsations.
Palpation: Trachea is central in postion.
Percussion: Resonant
Auscultation: Breath sounds are vescicular.
Abdomen examination:
Inspection: Shape is scaphoid.
Movements are equal.
Palpation: No tenderness
Normal temperature
No organomegaly.
Percussion: Normal.
Auscultation: Bowel sounds heard.
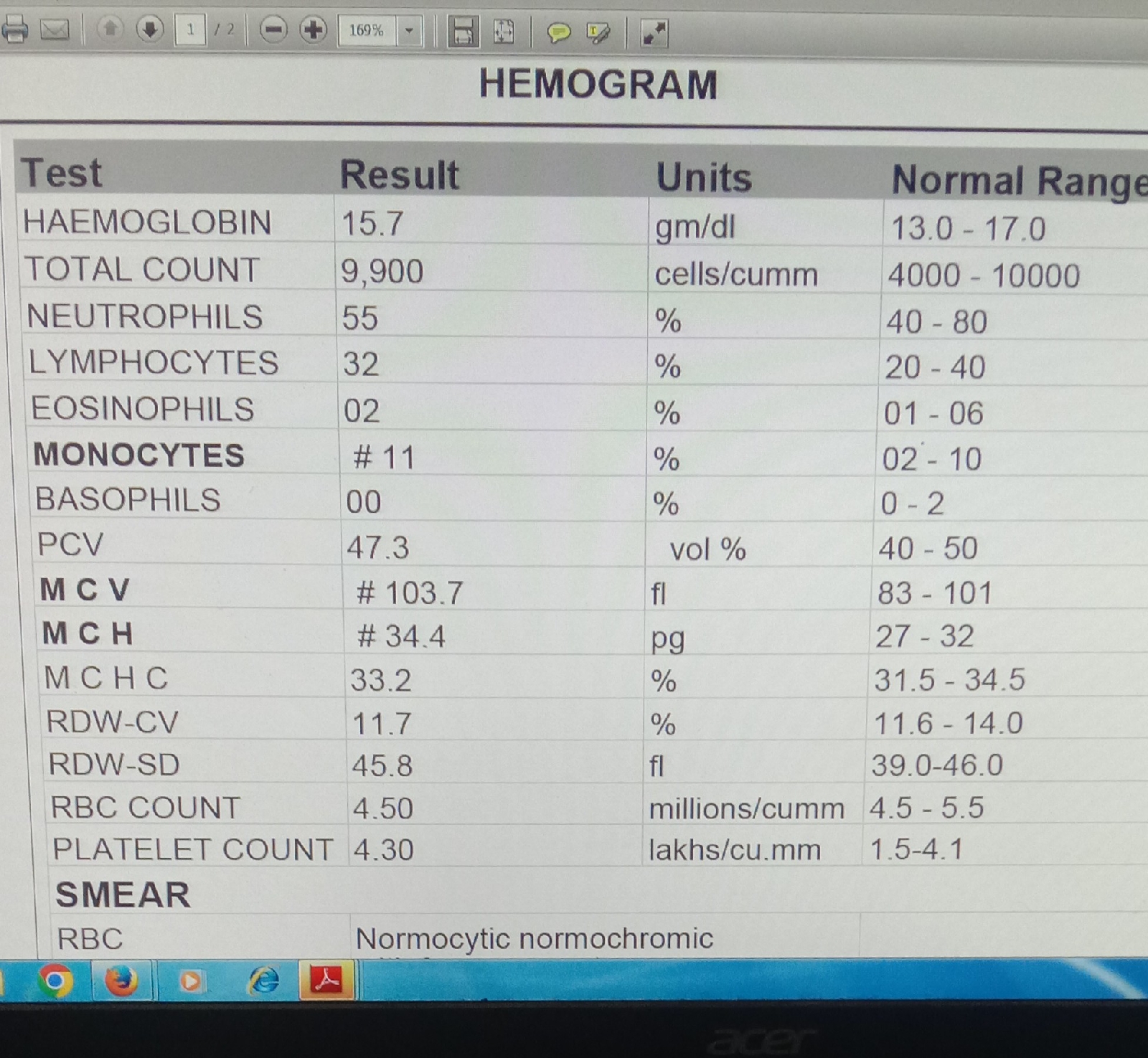
INVESTIGATIONS.
DIAGNOSIS:.
? ALCOHOL WITHDRAWL DELIRIUM
? ALCOHOL WITH DRAWL PSYCHOSIS
? ALCOHOL DEPENDENCE SYNDROME
TOBACCO DEPENDENCE SYNDROME WITH DIABETES MELLITUS AND HYPERTENSION.
TREATMENT:
1.IVF( NS,RL @ 75 ML/ HR
2. INJ THIAMINE 200 MG IV/ TID
3. INJ PAN 40 MG IV /OD/ BBF
4.TAB LORAZEPAM 2 MG PO/BD
5. INJ LORAZ 2 MG/ IM/ SOS
6.BP/ PR/ TEMP CHARTING 6 TH HRLY