A 40 year old male with shortness of breath.
This is an E log book to discuss our patient's de-identified health data shared after taking his guardian's signed informed consent. Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments in comment box are most welcomed
I have been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency i reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
SHORT CASE
Name.D.Shivani
Roll no.25
Hall ticket no: 1701006035
CASE SCENARIO
A 40 year old male pateint resident of bhongir painter by occupation presented to the old with the chief complaints of
Shortness of breath since 7 days.
Chest pain since 5 days
HISTORY OF PRESENTING ILLNESS.
patient was apparently asymptomatic 7 days back then he developed shortness of breath which was insidous in onset gradually proggrisve ( grade 1 to 2 MMRC) aggrevated on exertion and releived on rest.It is associated with chest pain which was pricking type non radiating .There was also history of loss of weight and appetite.no history of fever evng Rise of temperature,otthopnea,PND,Edema, palpitations, wheeze,chest tightness,cough,hemoptysis.
PAST HISTORY
No similar complaints in the past
Known case of diabetes since 3 yrs and is on tab metformin.
Not a known case of HTN asthama tb epilepsy.
PERSONAL HISTORY:
He is Married and Painter by occupation.
He consumes
Mixed diet
sleep is adequate ( but disturbed from past few days)
loss of appetite is present
bowel and bladder movements are regular
He used to Consume
Alcohol stopped 20years back ( 90ml per day)
Smoking from past 20years (10 cigarettes per day) but stopped 2years back.
FAMILY HISTORY:
No similar complaints in the family.
GENERAL EXAMINATION:
Patient is examined in a well lit room with adequate exposure, after taking the consent of the patient.
he is conscious, coherent and cooperative, moderately built and nourished.
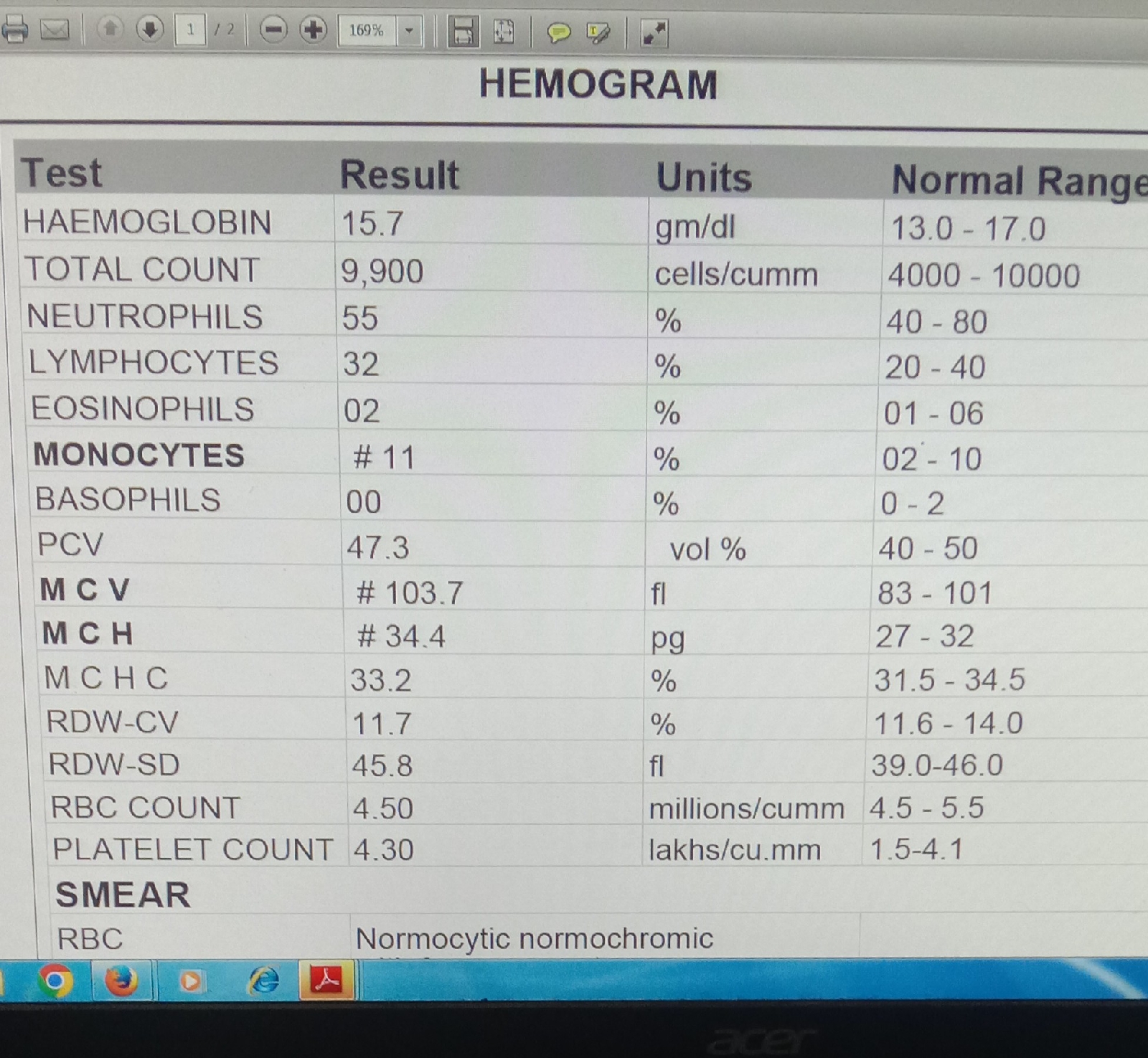
no signs of pallor, edema, icterus, cyanosis, clubbing, lymphadenopathy
VITALS:
Temperature : Afebrile
Pulse rate : 139beats/min
BP : 110/70 mm Hg
RR : 45 cpm
SpO2 : 91% at room air
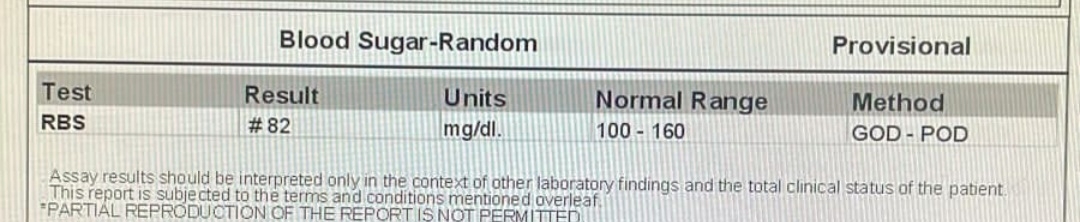
GRBS : 201mg/dl