A 48 year old male with fever and chest pain
This is online E-blog, to discuss our patient de-identified health data shared after taking her guardian's signed informed consent.
2. IVF NS , RL @ 75 ml/hr
3. 8 am 2 pm 8pm
Inj. HAI 6 U - 6 U
NPH 6 U 6 U 6 U
4. Inj. PAN 40 mg/iv/bd
5. Inj. Zofer 4mg /iv/tid
6. Inj. Augmentin 1.2gm /iv/tid
7. Tab. Azithro 500 mg po/od
8. Inj. Thiamine in 100 ml NS/iv/tid
9. Syp. Benadryl 5ml PO/TID
10. Inj. PCM 1g /iv/sos
11 Hourly GRBS charting.
12. Syp. Cremaffin 30 ml/po/HS
13. Inj. KCL 2 amp in 500 ml /HS/IV over 5 hrs
Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve the patients clinical problem with current best evidence based input.
This E-blog also reflects my patient's centred online learning portfolio.
I have been given this case to solve in an attempt to understand the topic of "Patient Clinical Data Analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
Following is the view of my case...
48 year old male Toddy climber by occupation came to the OPD with the chief complaints of
Fever since 7 days
Chest pain since 4 days
Shortness of breath since 4 days
Cough since 4 days.
HISTORY OF PRESENT ILLNESS:
patient was asymptomatic 7 days back then he developed fever which was sudden in onset high grade associated with chills . Patient also complained of shortness of breath 4 days was insidious in onset and gradually progressive. Cough was sudden in onset not associated with sputum aggrevated . Patient also complained of left sided chest pain Which aggrevated with cough.
Patient had one episode of vomiting which was non bilious non projectile food as contents . There is no history of headache abdominal pain , distention, headache , orthopnea PND.
Patient had similar complaints of fever 5 years back.He was hospitalized for the same. He was also diagnosed with diabetes and was on oral hypoglycemic drugs and discontinued the medication.
He was hospitalized about 5 to 6 times with similiar complaints due to heavy alcohol intake and was diagnosed with fatty liver and jaundice.
Patient had history of seizures 5 years back . Each episode lasted for about 5 minutes and associated with uprolling of eyes , and tongue biting and loss of consciousness. There was about 4-6 episodes in one year. Last episode was 2 years back.
He had also got affected with COVID 1and half year back and vaccinated with covishield ( one dose ).
PAST HISTORY:known case of Hypertension
, Cerebrovascular accident,asthama, epilepsy.
Known case of tuberculosis 4 yrs ago and was on ATT
PERSONAL HISTORY
DIET : Mixed
APPETITE : normal
SLEEP : adequate
BOWEL AND BLADDER MOVEMENTS : regular
ADDICTIONS: He is a chronic alcoholic since past 30 years and consumes about 300 ml per day
He was rehabilitated for about 1 year yet continued consuming alcohol.
FAMILY HISTORY: Not significant
GENERAL EXAMINATION.
Patient is conscious coherent and co operative well oriented to time place and person.
PALLOR : present
ICTERUS : absent
CYANOSIS : absent
CLUBBING : absent
LYMPHADENOPATHY : absent
EDEMA : absent
VITALS
BP : 130/90 mm hg
PULSE : 72bpm
RESPIRATORY RATE : 14/ min
SYSTEMIC EXAMINATION:
CARDIO VASCULAR SYSTEM: S1 S2 heard no murmurs.
RESPIRATORY SYSTEM:
INSPECTION:
SHAPE OF CHEST : bilaterally symmetrical
MOVEMENT OF CHEST : normal
POSITION OF TRACHEA: Central
EXPANSION OF CHEST : Normal
PALPATION; no local rise of temperature.
POSITION OF TRACHEA: central
APEX BEAT : felt in the 5 th intercostal space 1 cm medial to the midclavicular line.
VOCAL FREMITUS: increased in the infra mammary and interscapular areas
AUSCULTATION:
BREATH SOUNDS : decreased breath sounds on left side
Vocal resonance decreased in infra mammary inter scapular areas
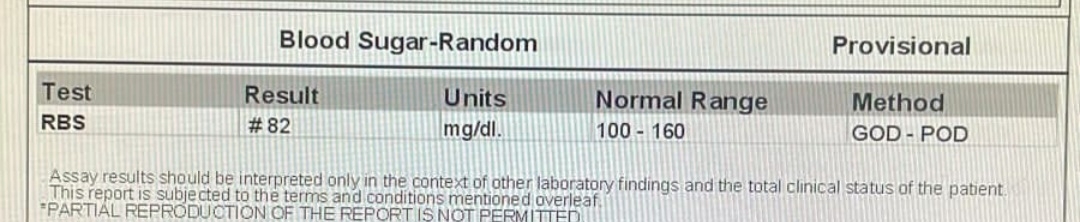
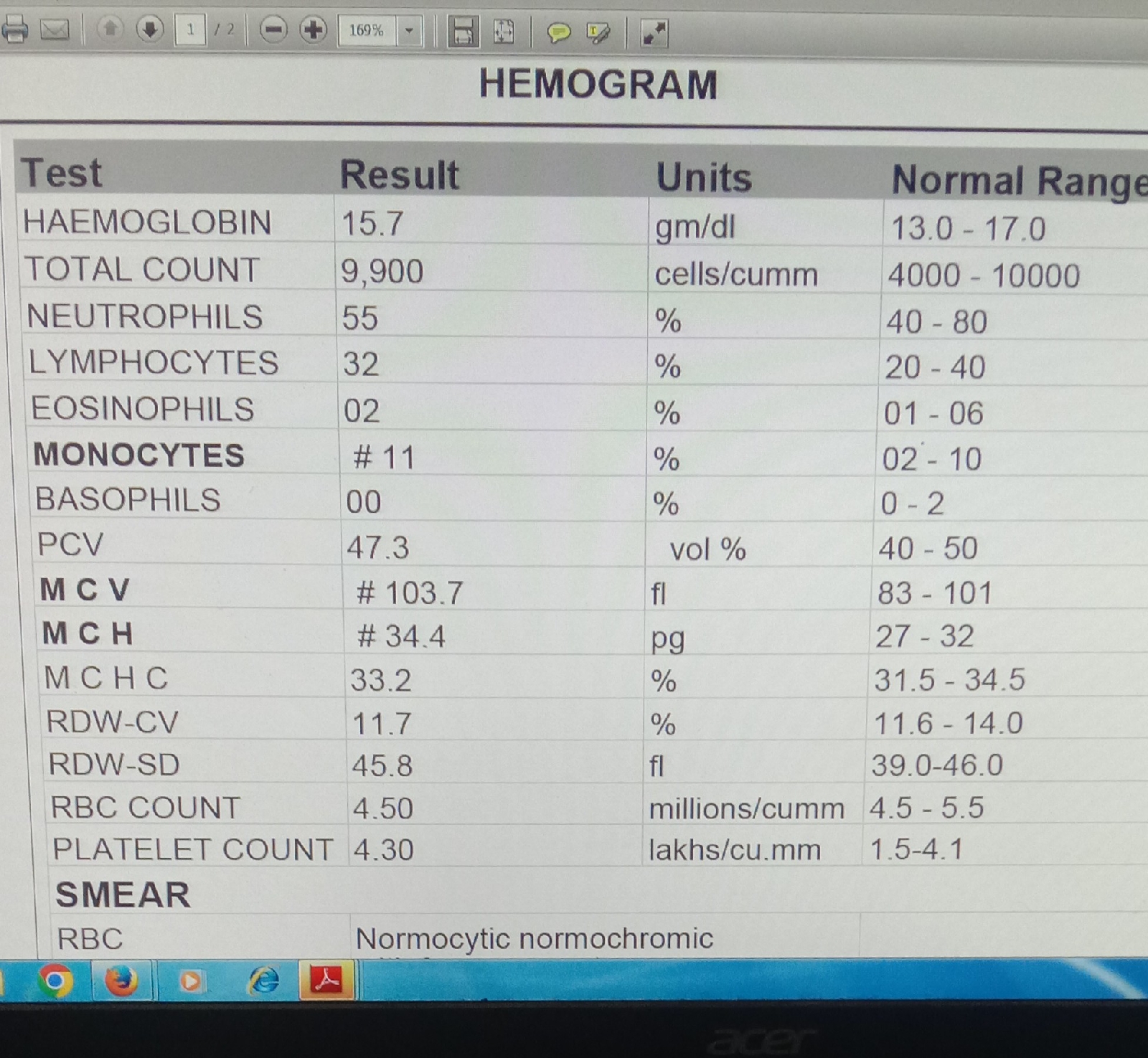
INVESTIGATIONS:
16/2/22.
1. Normal dietTREATMENT :
2. IVF NS , RL @ 75 ml/hr
3. 8 am 2 pm 8pm
Inj. HAI 6 U - 6 U
NPH 6 U 6 U 6 U
4. Inj. PAN 40 mg/iv/bd
5. Inj. Zofer 4mg /iv/tid
6. Inj. Augmentin 1.2gm /iv/tid
7. Tab. Azithro 500 mg po/od
8. Inj. Thiamine in 100 ml NS/iv/tid
9. Syp. Benadryl 5ml PO/TID
10. Inj. PCM 1g /iv/sos
11 Hourly GRBS charting.
12. Syp. Cremaffin 30 ml/po/HS
13. Inj. KCL 2 amp in 500 ml /HS/IV over 5 hrs
14. Inj. Tramadol in 100 ml NS over 30 mins