28 year old with seizures
This is online E-blog, to discuss our patient de-identified health data shared after taking her guardian's signed informed consent.
Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve the patients clinical problem with current best evidence based input.
This E-blog also reflects my patient's centred online learning portfolio.
I have been given this case to solve in an attempt to understand the topic of "Patient Clinical Data Analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan..
CASE SCENARIO:.
28 Year old male who is sales man by occupation presented to casualty with complaints of
Seizures - 15 days
Fever with chills and rigors -10 days
Cough - 10 days.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 11 months back then he noticed loss of weight about 10 kgs per month.
TIME LINE OF EVENTS:
Then he decided to remove Central line and shift to Avfistula , which was failed once , then he tried again so was not on dialysis for 3 months( september to december).
Then patient developed seizures 15 days back which was sudden In onset.It was a 3 episode seizure.
Each episode of seizure lasted for 3 to 5 minutes associated with frothing from mouth and rolling of eyes.
There was post ictal confusion for about 30 minutes for the first episode and about 10 to 15 minute after 2 nd and 3rd episode.
Not associated with involuntary micturition and biting of tongue.
Following 1 st episode he was taken to a nearby hospital and admitted for 3 days and discharged. Then patient developed 2 episode of seizure and he came back to hospital and was started on dialysis.
Patient also complained of shortness of breath which is insidious in onset and gradually progressive ( grade2) associated with dry cough , chills, decreased urine output and decreased appetite and chest pain since 10 days.
No history of burning micturition,hematuria,nausea, vomiting, loose stools,head ache confusion and loose stools.
PAST HISTORY :
•Not a known case of diabetes, asthma, TB , any CHD
FAMILY HISTORY
no significant family history
PERSONAL HISTORY
▪Diet-mixed
▪ Appetite-decreased
▪Bowel movements-Regular
▪Bladder movements-Decreased since 10 days
▪Sleep adequate
▪Habits- he was alcoholic and stopped since 8 months, and not a smoker
GENERAL EXAMINATION
▪Patient is conscious , coherent and cooperative and well oriented to time place
and person, moderately built and moderately nourished
- Pallor- present
-Icterus-absent
-Cyanosis-absent
-Clubbing-absent
-Lymphadenopathy-absent
-Edema-present ( right side)
VITALS
Temperature-98.6
Pulse rate-88 bpm
Respiratory rate-14 com
BP-160/100 mm h
Spo2-98%
GRBS-130 mg%
SYSTEMIC EXAMINATION
▪CVS-- s1 ,s2 heard no murmurs
• Respiratory system- pleural rub heard on right side.
• Abdomen- no tenderness seen, no. . palpable mass seen, not distended
▪CNS-
-Patient is conscious
-Speech -normal
-No signs of meningeal irritation
-SENSORY EXAMINATION,- touch, pain , vibration present
-No muscle wasting seen
-Tone of muscles is normal
REFLEXES:
DEEP TENDON ;. Right. Left
KNEE JERK. +2. +2
ANKLE JERK. +2. +2
BICEPS. +2. +2
TRICEPS. +2. +2
SUPINATOR. +2. +2
•Power : Right. Left
BICEPS. +5. +5
TRICEPS. +5. +5
FLEXORS OF KNEE. +5. +5
EXTENSORS OF KNEE+5. +5
FLEXORS OF HIP. +5. +5
EXTENSORS OF HIP. +5. +5
•Gait -normal
▪Coordination
- Finger nose test-able to perform
- knee heel test- able to operform
- Romberg sign- negative
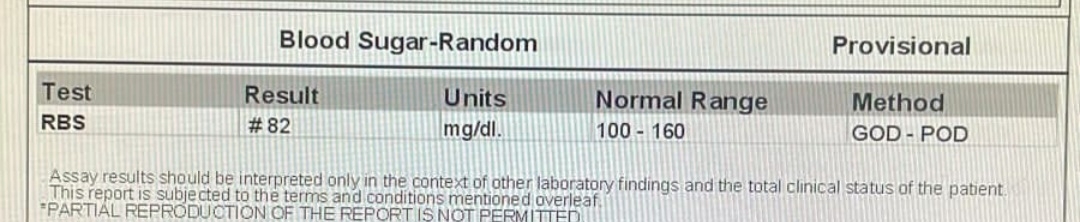
Investigation:22/12/21.
2d echo:
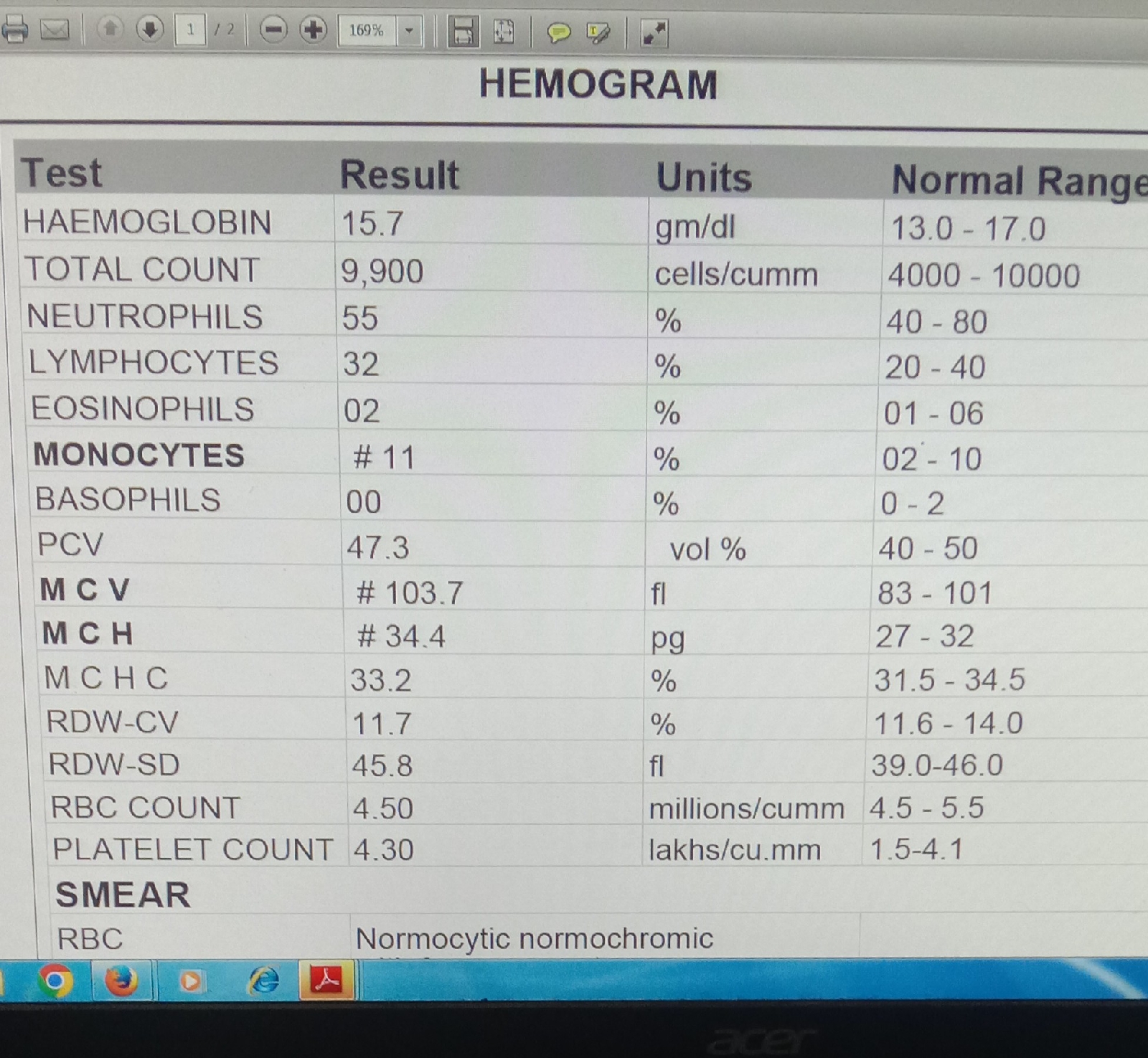
Liver function tests:CBP:
HB : 5.6gm/dl
TLC: 4000cells/mm³
PLT: 1.99 lakh/mm³
ABG
PH: 7.12
PCO2: 13.1
HCO3:6.9
RFT
UREA : 239mg/dl
CREATININE : 16.8
URIC ACID : 16.8
CALCIUM : 8.2
Na+: 145
K+: 5.7
Cl- 107
LFT
ALT : 08
ALP : 164.
23/12/21
24/12/21
25/12/21.
27/12/21
PROVISIONAL DIAGNOSIS:
UREMIC ENCEPHALOPATHY WITH CkD ON MHD WITH HYPERTENSIVE NEPHROPATHY.
TREATMENT:1) Fluid restriction( 1 ltr per day)
2)salt restriction( 2.4 g per day)
3)Tab NODOSIS( 550mg )PO/OD
4)Tab SHELCAL(500 mg) PO/OD
5)Tab OROFER Po/ OD..
6)Tab LASIX 40 mg PO / BD
7)TAB NICARDIA 10 mg PO/BD