A 74 year old female with fever and shortness of breath.
This is an elog book to discuss patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient
clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
CASE SCENARIO.
A 74 year old female came to the OPD with the chief complaints of
FEVER SINCE 4 DAYS
GENERALIZED WEAKNESS SINCE 4 DAYS
SHORTNESS OF BREATH SINCE 4 DAYS.
HISTORY OF PRESENT ILLNESS.
Patient was apparently asymptomatic 4 days back then she developed fever which was insidious in onset and intermittently progressive. Fever is associated with an episode of vomiting which subsided on its own.Fever is not associated with chills and rigor.
Patient also complained of generalized weakness since 4 days which was insidious in onset and gradually progressive.
Shortness of breath which was insidious in onset and gradually progressive. It was initially SOB at exertion but it progressed to SOB at rest.
Last year patient was having pericardial effusion for which she got treated.
PAST HISTORY.
Patient is a known case of hypothyroidism since 10 years and Is on medication.
Not a known case of diabetes hypertension asthma epilepsy.
PERSONAL HISTORY
DIET : mixed
SLEEP: adequate
APPETITE: normal
BOWEL AND BLADDER MOVEMENTS: regular
ADDICTIONS: No.
GENERAL PHYSICAL EXAMINATION.
Patient is conscious coherent cooperative well oriented to time place and person.Consent is taken and patient is examined in well lit room.
PALLOR : present
ICTERUS : absent
CYANOSIS : absent
CLUBBING : absent
LYMPHADENOPATHY : absent
EDEMA ; absent.
VITALS
PULSE: 76/min
BLOOD PRESSURE :140/90mm of hg
RESPIRATORY RATE :16 cycles/min
TEMPERATURE: febrile
SPO2: 98% at room air
SYSTEMIC EXAMINATION
CNS. Higher intellectual functions are normal.
CVS: S1 and S2 heard.
No murmers
RESPIRATORY SYSTEM: SOB( Grade3)
PER ABDOMEN: Normal, no tenderness and no organomegaly.
INVESTIGATIONS:
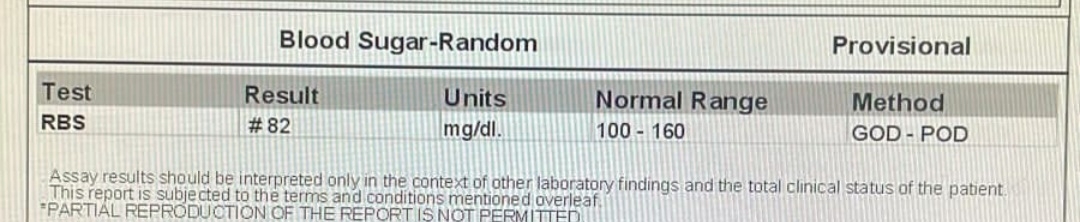
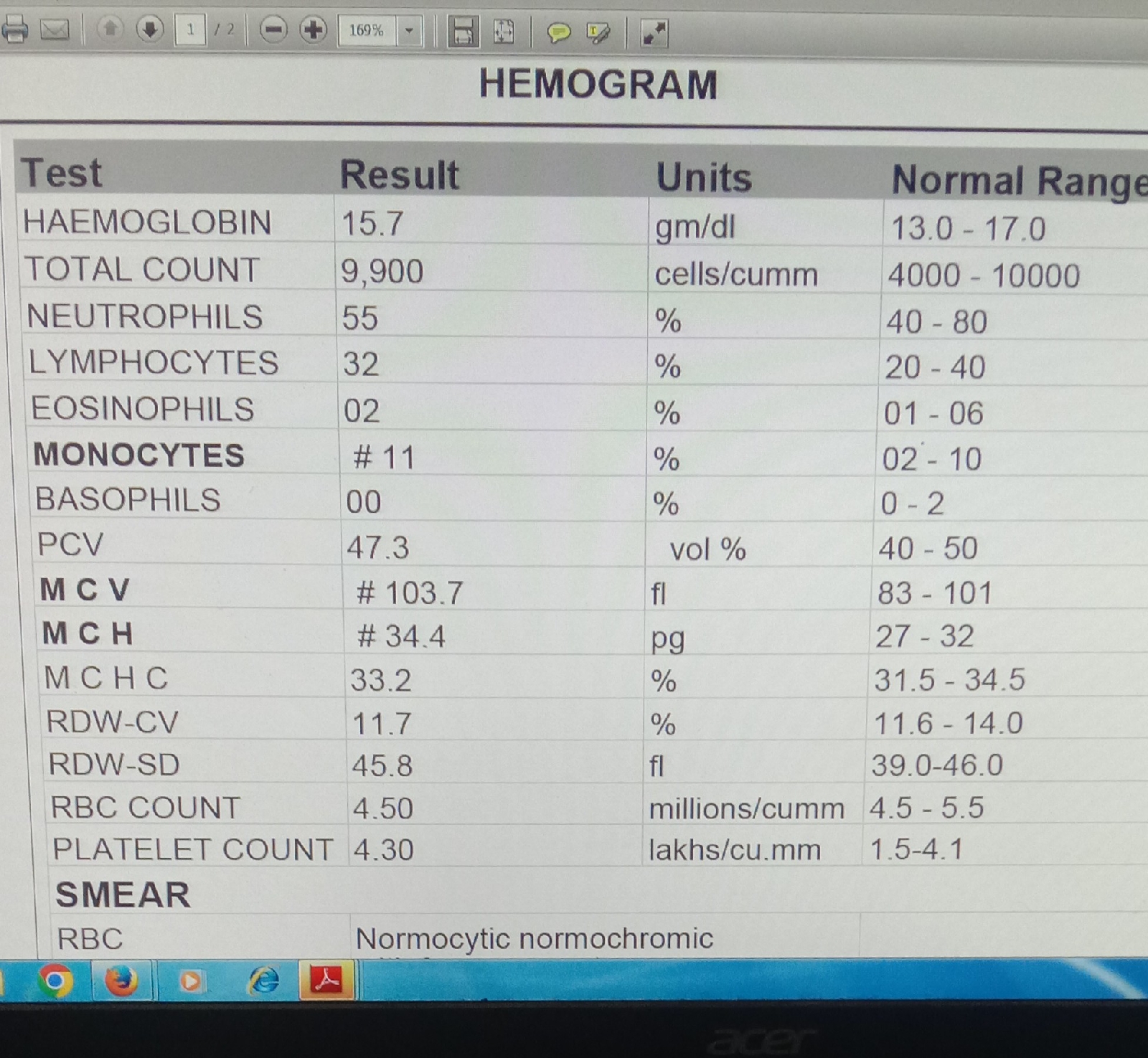
14/9/21
HEMOGRAM.
HEMOGRAM
PROVISIONAL DIAGNOSIS:
FEVER WITH THROMBOCYTOPENIA
URAEMIC ENCEPHALOPATHY
HEPATIC ENCEPHALOPATHY
TREATMENT
DAY1.
IVF normal saline@ 100 ml/Hr.
Inj pan 40 mgi.v od.
O2 inhalation
Monitor vitals and temperature.
Inj ceftriaxone 1g/i.v/ BD.
DAY 2
IVF @ 100ml/hr.
Inj pantop 40 MG/iv/ofinj Monocef 1gm/iv/Bd.
Inj Doxicycline100mg/i.v/BD.
Inj Falcigo 120 mg/i.v.
GRBS 6 TH hourly pre-meal.
BP/PR/ TEMPERATURE monitoring