A 65 year old male patient with abdominal pain.
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient
clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
CASE SCENARIO
A 65 YR old male patient came to the OPD on 28-8-2021 with chief complaints of
Pain in abdomen since 3 days constipation since 2 days.
HISTORY OF PRESENT ILLNESS
Patient was apparently asymptomatic then he developed pain in abdomen which was sudden onset and gradually progressive . Pain associated with an episode of vomiting which is non projectile nonbilious and water as its contents. Patient it also complained of constipation two days back. There is no fever headache giddiness etc. Patient is chronic alcoholic since 40 years and last intake was 3 days back.
Patient was kept under monitoring for 2 days . On 2/9 patient suddenly developed shortness of breath and then he was shifted to ICU. His pco2 levels were increased and oxygen saturation was decreased.
PAST HISTORY.
NO similar complaints in the past.
Not a known case of diabetes hypertension asthma epilepsy tuberculosis.
PERSONAL HISTORY.
DIET. mixed.
APPETITE. decreased
Sleep. Adequate
Bowel and bladder movements. Constipation
Addictions. Alcohol consumption 90ml per day.
GENERAL EXAMINATION.
patient is conscious coherent cooperative.
PALLOR. Absent
ICTERUS: present
CYANOSIS : absent
CLUBBING : absent
LYMPHADENOPATHY : absent
EDEMA : absent
VITALS
PULSE: 94/min
BP. 120/80mmof Hg
RR. 17/min
Temperature: Afebrile
SYSTEMIC EXAMINATION.
CVS. S1 S2HEARD.
no murmurs
Respiratory system. Normal vesicular breath sounds heard
Per abdomen. There is abdominal distension more in the epigastrium and hypochondrium. No palpable masses.liver and spleen Normal. No organomegaly.
CNS. NORMAL
INVESTIGATIONS
On EXAMINATION on 2/9/21
Pulse.89bpm
BP.140/90mm hg
CVS. S1 S2 +
P/A: soft non tender.
Pleural fluid was aspirated.
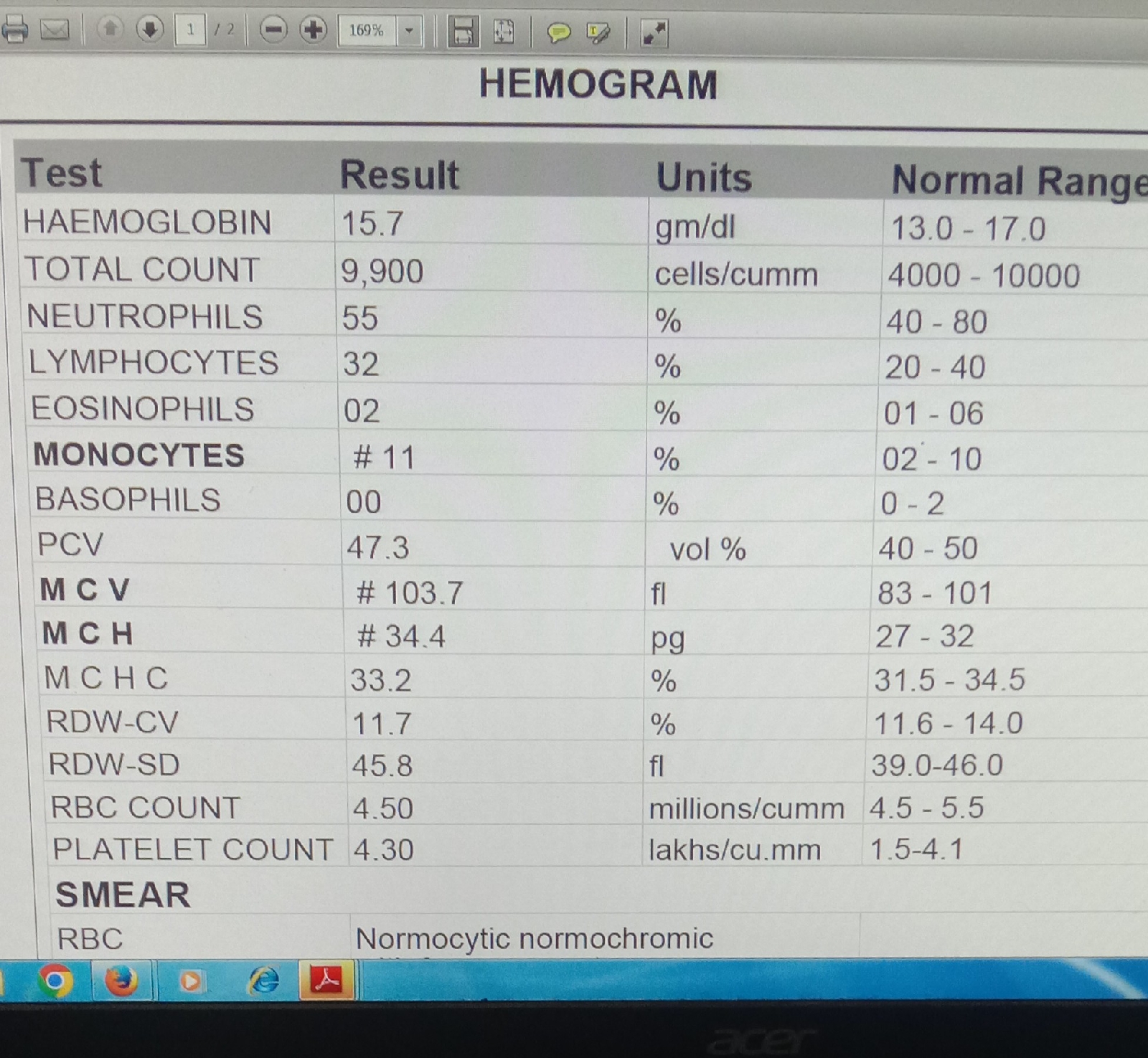
Sugars.103(60-90)
Protein-2.7(0-2.5)
LDH-200(230-460)
AMYLASE-111.5 .
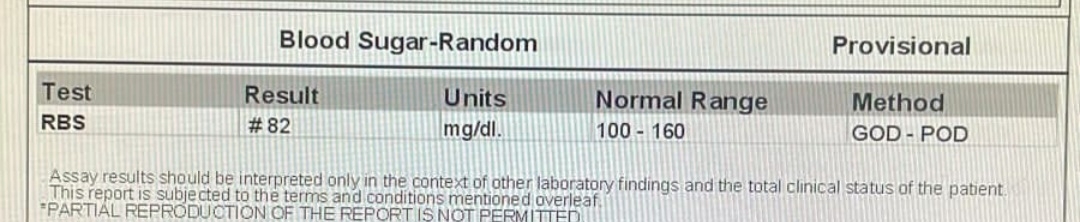
3/9/21 HEMOGRAM.
ABG
SOB DECREASED COMPARED TO YESTERDAY
BP.100/60mmhg
Pulse.82bpm
CVS.s1 S2 heard
Grbs: 136mg/dl.
PROVISIONAL DIAGNOSIS
ACUTE PANCREATITIS SECONDARY TO ALCOHOL.
TREATMENT.
29/8/21
NBM TILL FURTHER ORDERS.
IV FLUIDS@150ML/HR CONTINUES
INJ.PAN 40 MG I.V/BD.
INJ.TRAMADOL1 AMP IN 100ML NS I.V BD.
INJ .THIAMINE 1 AMP IN 100 ML I.V TID.
INJ.OPTINEUORON 1 AMP IN 100 ML NS / IV/OD.
BP PR TEMP SPO2 MONITORING.
30/8/21
ORAL FLUCOS IVF - NS @ 150 ml/ hr continuous.
INJ.PAN 40 MG I.V/ BD.
INJ.ZOFER 4MG IV.
INJ TRAMADOL 1 AMP IN 100 ML NS
I.V BD.
INJ THIAMINE 1 AMP in 100 ML I.V BD.
BP PR TEMP SPO2 MONITORING.