A 30 YEAR OLD PATIENT WITH FEVER AND LOOSE STOOLS.
This is an elog book to discuss patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient
clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
CASE SCENARIO.
A 30 Year old male patient lorry driver by occupation from tanga pally has come to the OPD with chief complaints of
Loose stools since 1 month
Fever since 20 days
Yellowish discoloration of eyes since 20 days.
Generalized weakness and SOB since 20 days.
HISTORY OF PRESENT ILLNESS.
Patient was a chronic alcoholic since 10 yrs.He consumes about 90-180ml/ day . 2 month ago patient only had binge intake without regular food intake.
Patient was apparently asymptomatic 1 month back . Then he has loose stools 3- 4 episodes per day which are watery and black associated with pain abdomen around umbilicus.there is decreased urine output with burning during micturition. Patient also complained of fever which was intermittent and low grade associated with weakness. Shortness of breath grade 2 which was insidious in onset.
No history of vomiting pedal edema orthopnea head ache
PAST HISTORY.
No similar complaints in the past.
Not a known case of diabetes, hypertension, asthama, epilepsy.
PERSONAL HISTORY.
DIET- vegetarian
APPETITE- decreased
SLEEP- adequate
BOWEL MOVEMENTS - loose stools.
BLADDER MOVEMENTS- burning micturition
ADDICTIONS- Chronic alcoholic
Stopped 1 month back
GENERAL EXAMINATION
Patient is conscious coherent cooperative well oriented to time place and person.
PALLOR- present
ICTERUS- present
CYANOSIS- absent
CLUBBING- absent
LYMPHADENOPATHY- absent
EDEMA - present
There is blackish discoloration of both hands since 1 year.
Tongue is hyper pigmented.
Knuckle is hyperpigmented.
VITALS
Temp- 98.7F
PR- 120BPM
BP-100/60mmhg
SPO2- 98%
SYSTEMIC EXAMINATION.
CVS: S1 and S 2 heard
No murmurs
RESPIRATORY SYSTEM: normal vesicular breath sounds heard.
pER ABDOMEN: no organomegaly
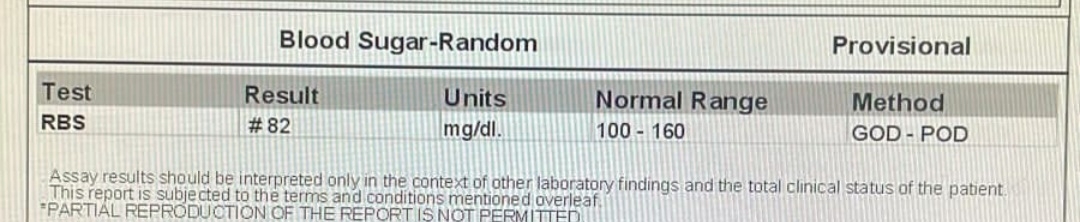
INVESTIGATIONS
DAY 1
Hb - 2.1
TLC-3500
PLT- 40000
PCV- 5.9
PT-17 sec.
APTT-35 SEC.
BT- 2 min 30 sec.
CT- 5 min
STOOL FOR OCCULT BLOOD- Positive.
RENAL FUNCTION TEST
UREA-27.
CREATININE-0.8
SERUM ELECTROLYTES
SODIUM-138
POTASSIUM- 4.1
CHLORIDE- 98
LIVER FUNCTION TEST
AST- 12
ALT- 10
ALP- 139
A/G- 1.5
TOTAL BILIRUBIN- 3.42
DIRECT BILIRUBIN-0.60
ALBUMIN-3.4
SERUM IRON- 70
LDH- 844
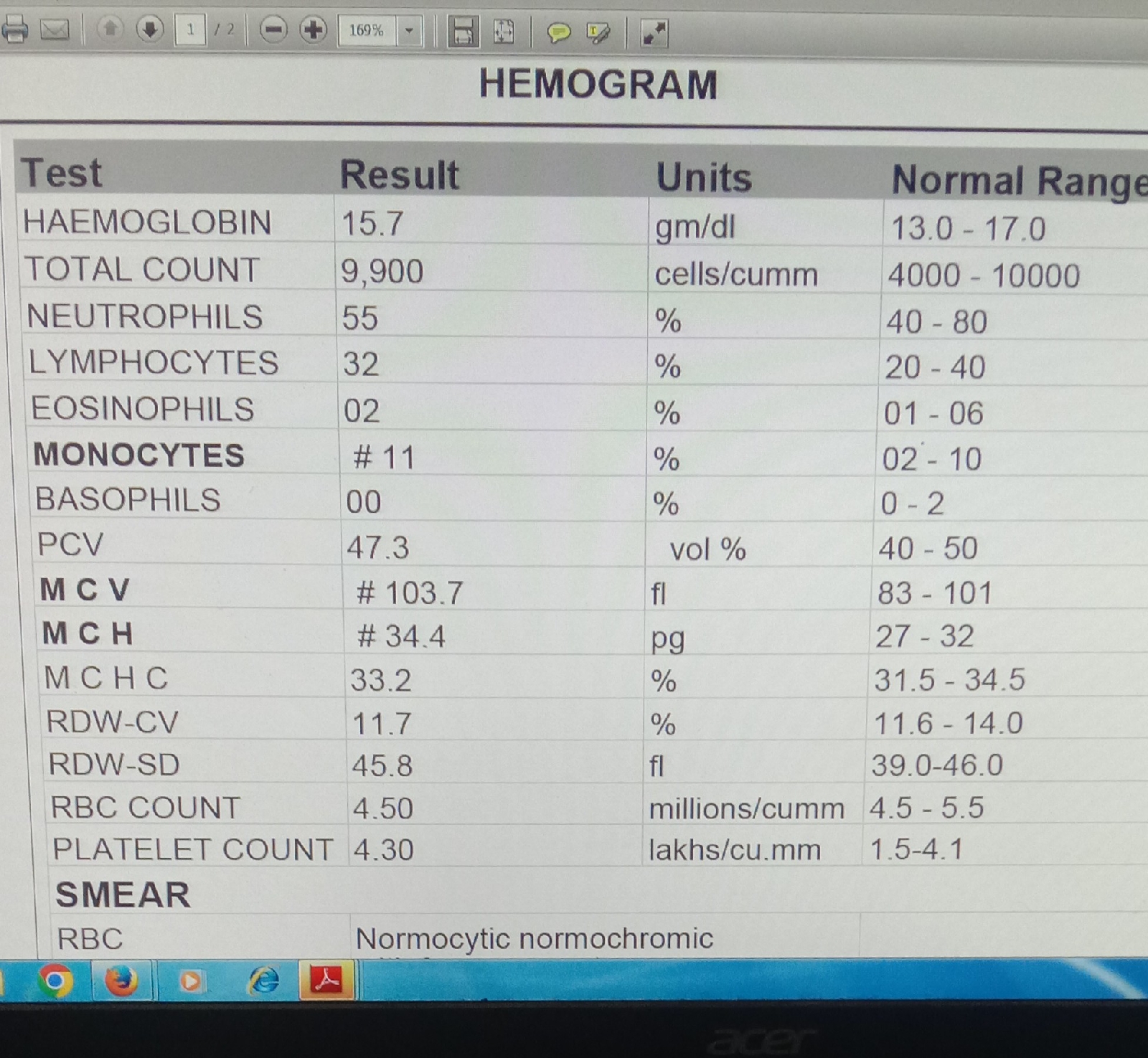
DAY 2
HEMOGRAM.
HB-3.3
TOTAL COUNT-3300
LYMPHOCYTES-51
MCH-33.
MCHC-35.1.
RBC COUNT- 1 LAKH
PLATE LETS- 15000
IMPRESSION: Anisopoikilocytosis with hypochromia
Decreased WBC with relative lymphocytosis.
SERUM ELECTROLYTE
sodium-138
Potassium-3.9
Chloride- 99
RENAL FUNCTION TEST
Urea-24.
Creatinine-0.8
2d ECHO.
PROVISIONAL DIAGNOSIS:
PANCYTOPENIA SECONDARY TO B12 DEFICIENCY.
TREATMENT
DAY 1
O/ E.
TEMP- Afebrile
BP- 110/60mmhg
SPO2- 98%
1. Inj vitcofol 1amp 1000mg/IM/daily for 1 week
2. Inj Thiamine 2 amp in 100ml NS/IV/ TID.
3. Inj PAN 40 MG/Iv/ od.
4. Inj ZOFER 4MG/I V/ sos
5. TAB PCM 650 mg/ po/ sos.
6. INJ. CEFTRIAXONE 1gm/ i.v/bd.
Monitor vitals.
8. GRBS Charting
DAY 2.
BP-100/50mmhg
PR- 80BPM
1. INJ Vitcofol 1 AMP 1000mgIM DAILY.
2. INJ PAN 20 MG IV/ SOS.
3. TAB PCM 650 mg po/ sos.
4. Inj Ceftriaxone 1 gm/ iv/ BD.
5. VITALS monitoring 4 th hrly.
6. STRICT I/O Charting
7. GRBS 8 th hrly