A 36 year old male with dyspnoea
D.Shivani
Roll no.25.
8 th semester
Date: 05 - 06 - 2021
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient
clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
CASE SCENARIO
A36 year old male from Nalgonda came to the OPD on 24-5-2021 with chief complaints of
. Productive cough since morning.
. Dyspnea since 11.AM at rest.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic then he developed cough which was insidious in onset progressive in nature. It was a productive type and non blood stain.
He also developed dyspnea which was insidious in onset and gradual in progression.
He was tested positive for covid-19 via rapid antigen test on 23-5-2021(HRCT CHEST CORADS- 25/25 with bilateral mild pleural effusion).
There is no history of loss of taste and smell, chest pain, vomiting, headache.
PAST HISTORY.
. There is no history of hypertension, diabetes, asthama, epilepsy, tuberculosis.
PERSONAL HISTORY:
.Diet: Mixed
.Appetite: Normal
.Sleep: Adequate
.Bowel and Bladder movements: regular
. Addictions: consumes alcohol occasionally.
.No allergies
FAMILY HISTORY:
Not significant
DRUG HISTORY:
Not significant
GENERAL EXAMINATION:
The Patient is examined with informed consent.Patient is conscious, coherent, cooperative,is well oriented to time, place and person.
. Pallor: Absent
. Icterus: Absent
. Cyanosis: Absent
. Clubbing: Absent
.Edema: Absent
. Lymphadenopathy: Absent.
VITALS
On the day of admission:
Pulse rate: 110 BPM
Spo2: 90%on 15 litres of O2 with NRBM mask
25-05-2021
Pulse rate:94 BPM
Spo2: 90% on 10litres of O2
SYSTEMIC EXAMINATION :
CVS - S1 and S2 heard
No added thrills,murmurs
RESPIRATORY SYSTEM ; Normal vesicular breath sounds heard
Dyspnoea: grade 4( NYHA GRADE)
PER ABDOMEN : soft, non tender, no organomegaly
CNS : intact.
INVESTIGATIONS:
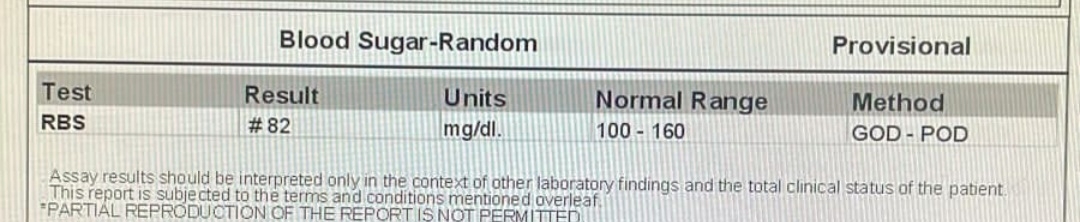
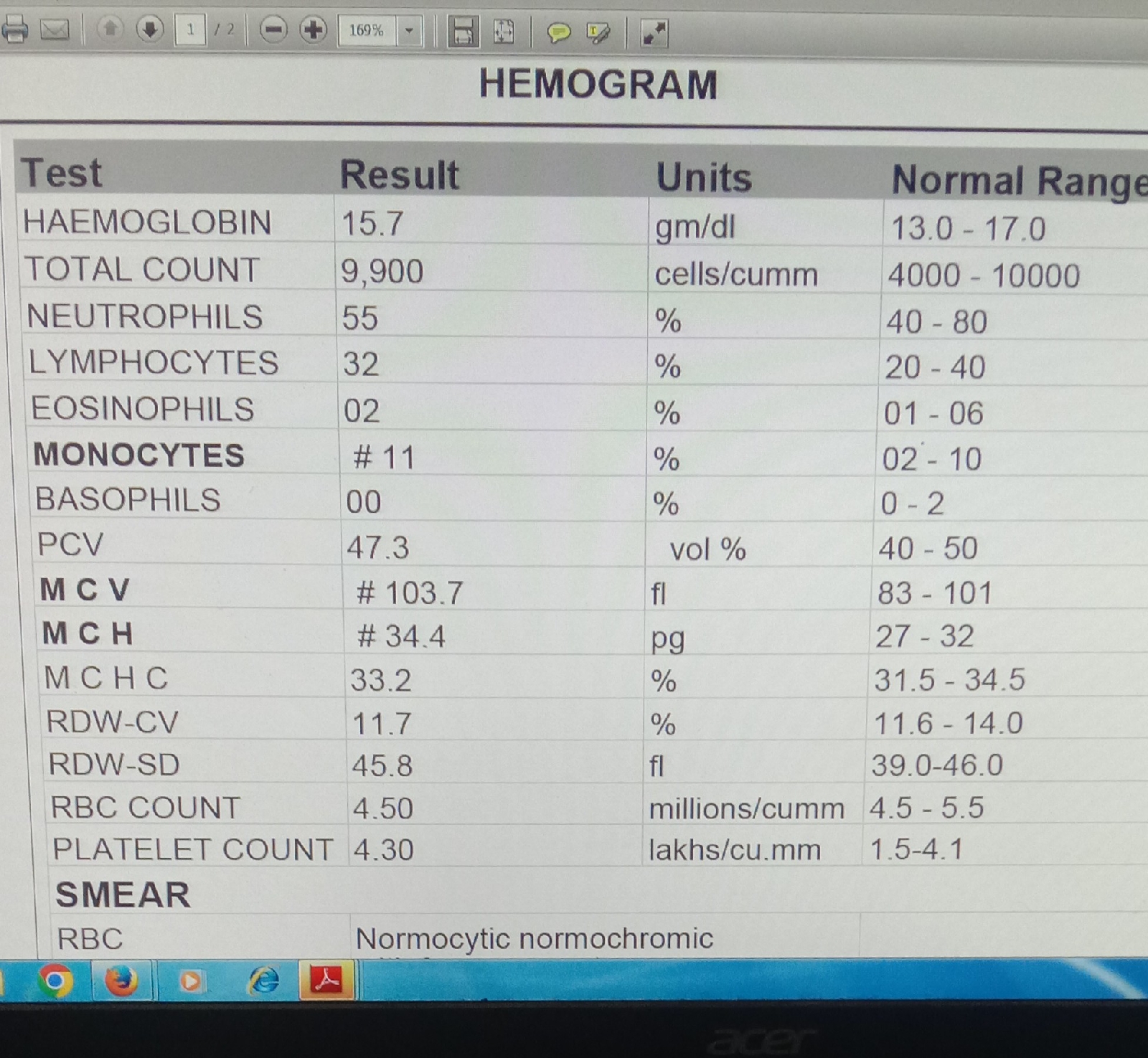
1.COMPLETE BLOOD PICTURE:
4. C- REACTIVE PROTEIN
5. FERRITIN
6. D- DIMER
7. HRCT :
PROVISIONAL DIAGNOSIS:
VIRAL PNEUMONIA SECONDARY TO COVID-19 INFECTION ( SEVERE)
TREATMENT REGIMEN.
24- 05- 2021
1.INJ . REMIDISVIR- 200 MG OD
2.INJ CEFTRIAXONE - 1gm/IV/BD
3.INJ METHYLPREDNISOLONE- 125 MG/IV/BD
4.INJ PAN-40MG / IV/OD
5.INJ CLEXANE - 40 MG/SC/OD
6.TAB LIMCEF- TID/ PO
7.TAB ZINCOVIT - OD/PO
8.NEB DUOLIN BUDICORT - TID
9.INJ NAC 60MG/ KG/ DAY IN 500 ML NS- OD
25 -05-2021
1.O2 SUPPLEMENTATION
2.FREQUENT CHANGE IN POSITION
3.INJ . REMIDISVIR- 100 MG OD
4.INJ CEFTRIAXONE - 1gm/IV/BD
5.INJ METHYLPREDNISOLONE- 125 MG/IV/BD
6.INJ PAN-40MG / IV/OD
7.INJ CLEXANE - 40 MG/SC/OD
8.TAB LIMCEF- TID/ PO
9.TAB ZINCOVIT - OD/PO
10.INJ NAC 60 MG/ KG/DAY IN 500 ML NS- OD
11.TAB INDOMETHACIN -25 MG OD
12.TAB ARIP/PRAZOLE- 5MG OD
13.INCENTIVE SPIROMETRY
14 BREATHING EXERCISES
15.TAB DOXYCYCLINE- 100 MG BD
16.TAB IVERMECTIN- 12 MG BD