GENERAL MEDICINE CASE DISCUSSION
D.Shivani
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient
clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan under guidance of Dr.Sai Charan sir.
CASE SCENARIO.
A 38 year old male patient came to the OPD on 17/05/2021 with chief complaints of
FEVER SINCE 14 DAYS
GENERALIZED BODY WEAKNESS SINCE 8 DAYS
SHORTNESS OF BREATH SINCE 7 DAYS
HISTORY OF PRESENT ILLNESS
Patient was apparently asymptomatic 14 days back then he developed
-Fever which was insidious in onset.Intermettent in nature not associated with chills and rigors and there were no aggrevating and releiving factors.
-Generalized body weakness which was insidious in onset gradual in progression .He was tested positive for rapid antigen covid on 4-05-2021(HRCT CHEST CORADS 6,CTSI 14/25) .
- He developed Grade 2 shortness of breath(NYHA CLASSIFICATION) 7 days back which was insidious in onset and gradual in progression.
There is no history of loss of taste and smell chest pain , vomiting , cough chest pain or head ache.
The patient got tested for covid-19 via RTPCR and was stated positive.
PAST HISTORY
- The patient is a K/C/O Hypertension since 3 years and is on medication.
- Not a K/C/O ;Diabetes,Asthma,Tuberculosis,and any other chronic illnesses.
- Diet : Mixed
- Appetite : Normal
- Sleep : Adequate
- Bowel and Bladder movements : Regular
- No Addictions
- No allergies
- Patient is on Anti-Hypertensive Treatment.
- Took 6 doses of remedesvir injection for covid -19 infection.

VIRAL PNEUMONIA SECONDARY TO COVID-19 INFECTION.
TREATMENT REGIMEN:
17/05/2021
O2 INHALATION TO MAINTAIN SPO2>90%
Iv fluids - 1 unit NS with 1 amp of optineuron @ 75ml/hr
INJ.PANTOP 40 MG/IV/OD
TAB.DEXAMETHASONE 4MG/PO/BD
TAB.LIMCEE/PO/OD
TAB.TELMA H(40/12.5)/PO/OD
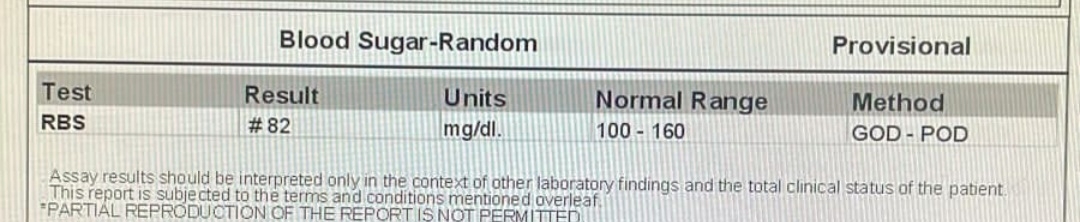
GRBS MONITORING 8TH HRLY
BP,PR,SPO2 monitoring
18/05/2021
O2 INHALATION TO MAINTAIN SPO2>90% ivfluids - 1 unit NS with 1 amp of optineuron @ 75ml/hr
INJ.PANTOP 40 MG/IV/OD
TAB.DEXAMETHASONE 4MG/PO/BD
TAB.MVT/TO/OD
TAB.LIMCEE/PO/OD
GRBS MONITORING 8TH HRLY
BP,PR,SPO2 monitoring.
19-05-2021
O2 INHALATION TO MAINTAIN SPO2>90%
Iv fluids - 1 unit NS with 1 amp of optineuron @ 75ml/hr
INJ.PANTOP 40 MG/IV/OD
TAB.DEXAMETHASONE 4MG/PO/BD
TAB.MVT/TO/OD
TAB.LIMCEE/PO/OD
GRBS MONITORING 8TH HRLY
BP,PR,SPO2 monitoring.
VITALS AT THE TIME OF DISCHARGE (19/05/2021)
PULSE :86BPM
BP: 130/60MM HG
Temperature:Afebrile
Spo2:99%on room air
ADVICE AT DISCHARGE
TAB PAN 40 MG/PO/1-0-0X 1WEEK
TAB MVT/PO/0-1-0 X 1WEEK
TAB LIMCEE /PO/0-1-0 X 1WEEK
TAB DOLO650MG/PO/SOS
TAB TELMA H(40/12.5)/PO/1-0-0X 1WEEK
SYP GRILLINCTUS /PO/10ML-10ML-10ML
INCENTIVE SPIROMETRY
Date of discharge: 19-05-2021(10:00AM)